What’s the connection?
The mouth is the gateway to the body’s digestive and respiratory tracts, making it essential to maintain oral health and guard the gateway from harmful invaders.
It’s normal for the mouth to have harmless bacteria, and saliva can naturally fight off small amounts of harmful bacteria that are present. However, lack of oral hygiene, hormonal changes, lack of saliva and genetic disorders can lead to the flourishing of harmful bacteria in the mouth that cause disease.
These harmful bacteria create plaque that builds on the teeth and infects the gums. Left unchecked, your mouth can develop Gingivitis, or a more serious gum infection, Periodontitis (Periodontal Disease).
Gum infections allow the bacteria to enter the bloodstream through the gums, forming plaque and blood clotting. Blood clots may restrict the flow of blood and lead to heart attack or stroke.
Oral infection may also contribute to:
- Endocarditis – an infection of the inner lining of your heart valves and chambers, (the endocardium). This usually occurs when bacteria, fungi or other germs from another part of your body, such as your mouth, spread through your bloodstream and attach to areas in the heart that have been damaged.
- Cardiovascular Disease – a class of diseases involving the heart or blood vessels, sometimes caused by plaque buildup thickening and stiffening artery walls, often leading to heart attack or stroke
- Pregnancy and Birth Complications – inflammation of the gums can trigger a series of tissue-destructive events that pass into blood circulation, and can cause premature birth and miscarriage.
- Pneumonia – the presence of oral pathogens associated with gum infection have been known to increase a patient’s risk of developing or escalating existing respiratory disease
- Memory Loss – infected gums can allow bacteria to enter the bloodstream and spread to the brain, causing inflammation and production of the toxic proteins that cause Alzheimer’s disease
- Weakened Immune System – Excess harmful bacteria in the gums can create a severe imbalance in the gums’ microbial community. This in turn weakens the immune system, leading to shortened life expectancy.
Further Complications:
If the gum infection progresses to Advanced Periodontitis, the teeth may become loose and fall out, or cause serious pain and need to be extracted. When teeth are lost, this further escalates the impact of oral health on overall health:
- Tooth loss may require a person to restrict themself to a soft food diet, causing a risk of malnutrition, which can lead to greater risk of disease. Those that switch to a denture may lose appetite due to coverage of the palate, escalating nutrition problems.
- Many who lose teeth begin to refrain from smiling and socializing, for fear or embarrassment. As smiling and socializing are integral to mental health, refraining from these over long periods of time can have a negative impact on the brain.
How to protect against oral infection:
- Brushing and flossing, as recommended by dentists, is the best way to prevent the spread of bacteria and plaque in the mouth. Mouthwash also helps rinse out bacteria that may have been left over while brushing.
- Visiting the dentist regularly (twice a year) allows a professional to assess the current state of your oral health and clean any build-up that is difficult to remove through simply brushing and flossing.
- Some medicines have a side effect of inhibiting saliva production. As saliva helps fight bacteria, you may benefit from speaking with your doctor about switching medications if you experience dry mouth.
How to treat Gum Disease that has already developed:
Gum disease in its early stages can sometimes be maintained using the solutions mentioned above. If gum disease progresses to an advanced stage (Advanced Periodontitis), however, the infection has likely already spread below the gum line and around the roots of the teeth. In these cases, surgical action may be necessary.
Those with Advanced Periodontal Disease have likely already lost teeth or are in progress of losing them. To remove the infection, an oral surgeon may need to extract the affected teeth and make an incision in the gums to access the underlying infection and eradicate it.
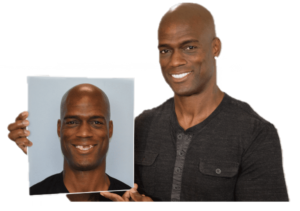
Patients who undergo this procedure may use a denture to replace extracted teeth, but the ideal solution is to have dental implants placed instead. This is because:
- A denture permanently restricts its wearer to a soft diet, which can prevent them from ingesting needed ingredients from harder-to-chew foods.
- The denture’s coverage of the palate can also cause a loss in appetite and further complicate nutrition problems.
- Gaps between the denture and the gums leave room for food to become lodged and bacteria to accumulate
- Dentures don’t provide a replacement for the root of extracted teeth. This leaves the jaw bone unsupported, causing it to deteriorate.
Dental Implants, on the other hand, can restore up to 85% of original bite force (compared to dentures that restore up to 25%), allowing the recipient to eat normal food. They also act as the root of a tooth to reinforce the jawbone and maintain its integrity.